Cataract surgery
Prof. Dr. Abela-Formanek - Ophthalmologist for ophthalmology and optometry in Vienna
Cataract surgery
Cataracts are the most common cause of visual impairment at around the age of 60.
A cataract causes the lens to become cloudy when it is typically clear. Cataracts can eventually affect vision. This procedure is considered to be very common and generally safe. Nowadays, cataract surgery not only focuses on replacing the lens, but also corrects existing refractive errors, such as nearsightedness, farsightedness and astigmatism.
For a preliminary examination and planning of a cataract surgery, please make an appointment in the practice!
Focus on your eye health
Prof. Dr. Abela-Formanek looks back upon more than 25 years of experience in eye surgery and is considered an absolute expert in her field.
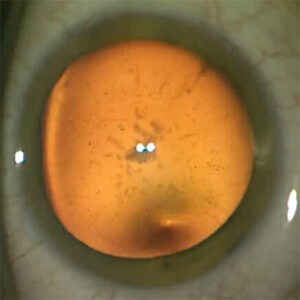
What is a cataract?
In cataracts the lens of the eye is clouded (cataracta complicata). Clouding of the human lens often develops very slowly over several years.
The causes: One of the most common causes for the development of cataracts is the natural aging process. Over the years, the metabolism of the lens slows down and as a result the lens becomes harder and loses its elasticity. Over time, vision impairment occurs due to lens opacification. Other causes for the accelerated development of a cataract can be attributed to various factors, e.g. other eye diseases (uveitis, high myopia), traumatic cataract (eye bruise, eye perforation), strong UV radiation, metabolic diseases (diabetes mellitus), chronic cortisone therapy, chemotherapy or Radiotherapy.
How do you notice cataracts yourself? Cataract symptoms develop slowly and can hinder daily activities when advanced. Below are some signs you can look out for:
- blurred vision
- glare
- Difficulty with night vision
- altered color perception
- frequent changes in glasses strength
- mono-ocular double vision
- Changes in contrast vision
The diagnosis: Progress can be determined using an eye test and an eye examination in the office. The anterior chamber, the cornea, the lens with all its layers, the vitreous body and the retina are examined. The eye is examined at the slit lamp to determine whether the lens is the only cause of the visual impairment. Precise measurements of eye length and corneal curvature are taken. An assessment is then made as to which lens should be implanted. After a consultation, it will be determined whether the operation should also correct a refractive error. After the information has been given, the patient has time to think before agreeing to an operation date and, if necessary, ordering a lens.
Eye length measurement before cataract surgery
IOL Master 700
This high-precision device measures the axial length of the eye, which is crucial for calculating the correct artificial lens power for cataract surgery. The measurement is non-contact and completely painless and usually takes only a few minutes.
This new device uses imaging OCT technology (SWEPT Source Biometry) and enables precise measurement of the length of the eye, even in the case of dense cataracts, including the measurement of the curvature of the cornea.
Answers to the most frequently asked questions about cataract surgery
The time-point for cataract surgery depends on a few factors. What must be taken into account is the extent to which the symptoms affect the patient's quality of life.
Cataract surgery should be considered if the following symptoms apply:
- Impaired visual acuity: If the deterioration in visual acuity caused by the cataract causes you to have difficulty reading, driving, or recognizing faces.
- Limitation of activities: If the cataract affects your ability to carry out everyday activities safely and comfortably, such as climbing stairs, cooking, or shopping.
- Increased glare: If you become increasingly sensitive to glare and it affects your activities such as driving and your safety.
- Worsening night vision: If you have difficulty seeing in low light, it may be a sign that a cataract is affecting your night vision.
- Altered color perception: If your color perception is affected by the cataract and this affects your daily tasks.
- Advanced cataract: When the view of the retina is so advanced that it makes possible diagnosis and treatment of retinal diseases impossible.
Before an operation takes place, a preliminary examination in the office is necessary. The eyes are thoroughly examined and measured and an assessment is made as to which lens should be implanted. After a consultation, it will be determined whether the operation should also correct a refractive error. The information sheet about the operation and, if applicable, the anesthesia procedure will be handed out. The majority of operations are treated in an outpatient hospital using topical anesthesia.
Other regularly prescribed drops (e.g. for glaucoma therapy) can be used as usual until the day of the operation.
Phacoemulsification of the cataract is the most common procedure for removing the lens.
It begins with local anesthesia of the eye using eye drops. Access to the eye is achieved through a 2.4 mm corneal microincision.
The lens capsule is then opened. Using high-frequency ultrasound vibrations (phacoemulsification), the cloudy lens is crushed and sucked out. What remains is an empty capsular bag into which a new artificial lens is inserted. The corneal microincision is elf sealing. An additional stitch is seldomly necessary.
It is particularly important to protect your eyes in the first few days after the operation. A transparent protective shell will be provided to you for this purpose. You should only wear it at night for 2-3 days. This is for safety reasons to avoid unwanted rubbing on the eye.
You will be prescribed eye drops that have an anti-inflammatory effect. It is important to take these drops reliably to promote the healing process.
After the operation, you can wash your face gently with your eyes closed and clean water. However, note that you should not rub the eye and avoid direct contact with contaminated water, shampoo or soap.
Driving is only permitted after a postoperative ophthalmological examination and a vision test. You can be active again after 3 weeks.
Cataract surgery is a very common, routine procedure and, thanks to the modern operation method, is associated with few complications. As with any surgical procedure, there can be undesirable effects.
- Deviation of the target refraction +/- 1 diopter in 10% of cases
- Capsule rupture <1%
- Infection in the eye (endophthalmitis) - 0.03%
- Post-cataract - 2-7 years postoperatively
- Retinal detachment - very rare
- Bleeding - very rare
During cataract surgery it is possible to correct both nearsightedness and farsightedness. Modern special lenses can also correct astigmatism. After the procedure, in most cases you will no longer need glasses for distance vision, but you will need reading glasses.
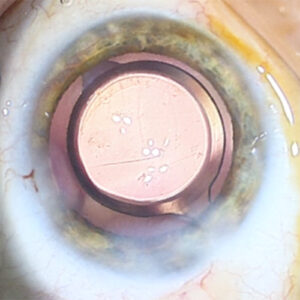
In some cases, vision may deteriorate again; this is known as an aftercataract. During routine cataract surgery, the cloudy lens is replaced with a new artificial lens; the lens capsule remains in place. This keeps the artificial lens in the correct position. In the case of a secondary cataract, the posterior capsule layer becomes opacified. The secondary cataract can be permanently eliminated through a short and painless laser procedure.
Special lenses
Intraocular lenses, also known as IOLs, are artificial lenses made of different materials. There are different types of intraocular lenses, all of which are well tolerated and can be worn for life, including acrylic (hydrophobic and hydrophilic lenses) and silicone (hydrophobic lenses) lens.
The right intraocular lens depends on various factors and your individual needs. I would be happy to advise you personally on which lens suits you best.
Astigmatism of over 1.5 diopters can be corrected intraoperatively using special intraocular lenses with built-in cylinder correction. Accurate measurement of the cornea with a corneal topographer is essential for the correct calculation and ordering of the lens.
Have the property of improved depth of vision. Patients can see up close at a distance of approximately 50 - 60 cm, slightly better than with monofocal lenses. Wearing reading glasses is often necessary in some situations.
Multifocal lenses have the advantage of allowing you to see both far and near. The light is refracted into different refraction points, which leads to a reduction in contrast sensitivity and the appearance of light phenomena. Patients see halos around light sources. Not every patient is suitable for implanting this lens.
Would you like to make an appointment or do you have questions about operations?
Give us a call. Dr. Abela-Formanek will be happy to answer your questions!